Abstract
Introduction: The first direct oral anticoagulant (DOAC) agents were approved for pediatric use in 2021. These have quickly gained favor over traditional anticoagulants among many hematologists and patients due to oral availability, favorable risk profile, and elimination of the need for frequent lab monitoring. This study aims to evaluate trends in DOAC use among pediatric patients with new venous thrombotic events (VTE) and patient-level and hospital-level factors associated with their selection.
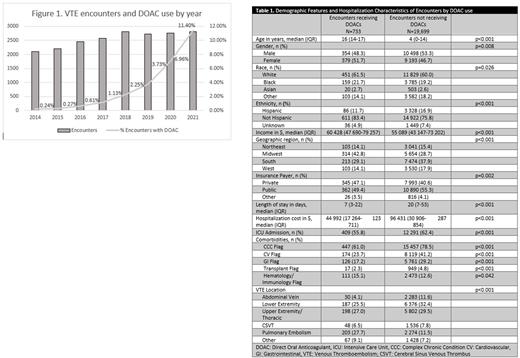
Methods: This retrospective study used data from the Pediatric Health Information System (PHIS), an administrative database of >50 US children's hospitals. We included initial inpatient encounters from 2014-2021 for pediatric patients (age <18). The visit required an ICD9 or ICD10 code for an acute thrombotic event and medication charge for one of the following anticoagulation agents: dabigatran, edoxaban, rivaroxaban, apixaban, betrixaban, low molecular weight heparin (LMWH), or warfarin. We included only the first encounter for each patient which met these criteria. We compared characteristics of patients who received DOACs to those who did not through descriptive and statistical analysis, and utilized multivariate regression to evaluate factors associated with DOAC selection.
Results: In 20,432 cases of new VTE, DOACs were administered in 733 encounters (3.59%). Rivaroxaban was the most administered (71.9% of DOAC use), followed by apixaban. DOAC use increased over time, it was prescribed in 0.24% of the encounters in 2014 up to 11.4% of the encounters in 2021. DOACs were first only administered to grade school age children (5-12 years) in 2016 and then moved to younger groups in 2019. Patients who received DOAC agents had a greater median age (16 vs 4 years, p<0.001), were more commonly female (51.7% vs 46.7%, p=0.008), had greater median income ($60,428 vs $55,089, p<0.001), and were more likely to carry private insurance (47.1% vs 40.6%, p=0.002). Geographic variation was also observed, with midwest hospitals prescribing DOACs more often than in the south and west (5.5% vs 2.8%). Patients who received DOACs during their admission had a shorter median duration of hospitalization, lower hospitalization costs, and were less likely to have a complex chronic condition (all comparisons were statistically significant). DOACs were most prescribed in cases of pulmonary embolism (8.2% of encounters carrying ICD code for pulmonary embolism). On multivariate regression analysis including age, gender, race, ethnicity, insurance payor, income, and geographic region, only age, income and geographic region remained statistically significant predictors of DOAC use (p<0.05).
Conclusion: This abstract describes the increase in DOAC usage over time. The decision to prescribe a DOAC agent appears to be affected by patient age, medical co-morbidities and income. The data presented suggests the presence of prescription trends that may not be based on clinical evidence. A better understanding of the safety and efficacy of DOAC agents in pediatric patients and education of pediatric hematology providers is necessary.
Disclosures
No relevant conflicts of interest to declare.
Author notes
∗Asterisk with author names denotes non-ASH members.